Our adoption journey has been so complicated medically that it is hard to know where to start and what to include, but here is a snippet. I hope it will help you as you make a decision for adoption.
My husband Chris and I had been married 16 years and had three beautiful biological boys when I felt the call to adopt. It wasn’t the first pull toward adoption, but it was the first time that we both felt we were ready for the financial and emotional stretching that an adoption would require.
We didn’t want to start all over again with a baby since our kids were already 5, 10 and 12, so we started look at “older child” adoption, between the ages of 3 and 5, with the child being at least one year younger than our youngest. We wanted a girl, because we had three biological boys and we chose cleft lip/palate, minor heart condition and club feet as conditions we thought we could handle. Significant developmental delays were not part of our list.
When we received Grace’s file, in June 2012, we read through all the details before we looked at her picture so we wouldn’t be swayed by a cute face whose medical needs would be too great for us. Everything seemed perfect. She was almost a year younger than our youngest. She was very tiny. Her lip had been repaired at age 1, and she had just had her palate repaired the summer before. We were happy at the time that both those surgeries had been completed, because that meant we wouldn’t have to start our journey with her in surgery, and we expected that she might not need another for several years. Her head size was listed as small, but when we finally looked at her pictures, she didn’t look disproportional, just tiny overall. And those measurements are often wrong, we knew. That evening, we both said ‘Yes, that is our girl’, and we started to move heaven and earth to bring her home.
Five months later we met our girl in Guangzhou, China. She was very cute and quite tiny (24 pounds at age 5.5), with a very odd, hollowly sound to her voice. The orphanage showed us how to stick a rolled up piece of toilet paper in her nose “so she could breathe at night”. She would not let us do it and spent the night alternately sleeping and gasping for breath. We emailed the cleft clinic the next morning to set up an appointment directly upon our return. A few days later when she was more comfortable with us, we were able to play the game where you sit them on your lap and lay them backwards toward the floor and pull them back up again. Once she was enjoying it and laughing, we could clearly see what we feared; her palate was open the whole way up to her nasal cavities.
Thus began our journey to close her palate – three years in and it continues today. We were home November 8th, 2012 and her first surgery was six weeks later. It was then that her US surgeon confirmed that there had been a surgery in China to close her palate that had in fact severed both of her palatal arteries, a major, life-altering fail. She was the worst case our surgeon had ever worked on or reviewed because of the damage done in China.
Her first surgery home failed because all of the tissue on the roof of her mouth was dead and could not heal together without sufficient blood flow. A second, slightly more complicated surgery in April also failed. June saw her in surgery again, this time for her nose and lip – to open it up, and reshape the nose so she could breathe better, especially at night, and to remove extra tissue below her nose. July brought another procedure to care for 13 cavity filled teeth, including many crowns. Four times under anesthesia in eight months; it was more than we had ever imagined. We are thankful our state has her covered under it’s disability policy as a second to our primary insurance. The financial ramifications could have been debilitating.
After almost a year with no surgery, another attempt was made to close her palate in July 2014. This involved an incision across the top of her head from ear to ear, cutting out her temporal muscle, cutting out her cheekbone, tunneling the muscle through the space made by the missing cheekbone and sewing that muscle on to the roof of her mouth, and then replacing the cheekbone and stitching her up. It was terrible and terrifying, and then it failed, like all the others. We were devastated to have put her through that to no great avail. A decision was eventually made to halt all surgeries for a period of time and try an obturator to close the palate artificially, to allow her some healing and growth.

She is now 8.5 and in first grade, having completed kindergarten twice. She is still tiny so she doesn’t stand out size-wise. She is diagnosed with microcephaly, a genetic difference in chromosomes 13 and 15, severe ADHD and was recently given an IQ of 73. She is, however, learning to read and learning to do basic math. It is not easy. She has to work hard at everything and requires a great deal of patience from teachers and caregivers.
Her language skills are greatly delayed compared to her non-cleft adopted cohorts, but she is able to get most of her needs met and most of her points made. She loves music and has recently started piano lessons, and although, as with everything, it is a bit of a struggle, she is doing remarkably well. We are prayerful that this will be helpful in healing and growing some of those brain pathways that she needs for higher level thinking.

We also recently removed all dairy products from her diet on the advice of a developmental pediatrician. So far, it seems to be clearing some of what he would term “brain fog” or “caseinomorphine” that stems from her intolerance to the dairy we had been feeding her for three years while trying to put some weight on her.
To close, I can’t be sure what is causing her learning delays. Is it the microcephaly, the significant language delay due to having an open, unrepaired cleft for 6 years, genetic issues, a combination of all three or something else? We don’t know and may never know.
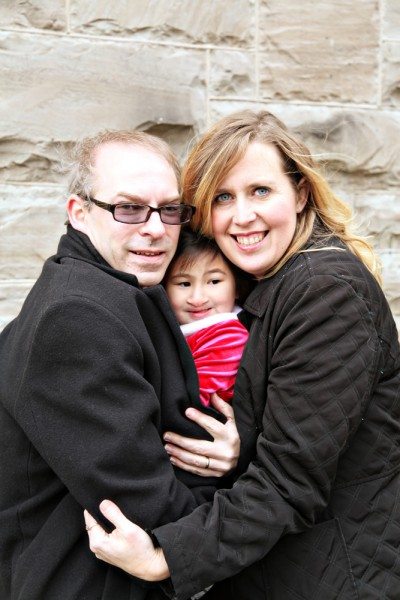
What we do know, is that she is loved. She is a cherished daughter, sister, granddaughter, niece, and daughter of the King. She has love for everyone around her and we are helping her to heal, emotionally and physically. She has great potential to be a loving wife, a loyal friend, a lover of Jesus, and an independent adult. She is teaching us to be more patient, more loving, more gentle, and more like Jesus. As hard as this has been, I wouldn’t trade our girl for anything. I cannot wait to see what God has planned for her.
– guest post by Christine

























Grace, you are a Daughter of The King! A precious gem. I am so happy that you have a family that loves you and fights hard to get you everything you need to become healthy. I will be praying for you and for your family. Thank You, Christine, for sharing your beautiful daughter.
You mentioned taking Grace off of dairy products. There is a book that has been life changing for me. It’s called the Wheat Belly Diet. Grace does to need to lose weight, but the information regarding grains and sugar and how they effect all of us is really amazing. There is a group on FB, as well. I hope it will give you some ideas to discuss with Grace’s doctors.
God Bless you. – Jo