My son has Cerebral Palsy.
Mild Right Hemiplegic Cerebral Palsy to be specific, which means only the right side of his body is affected.
If you see him running by on the playground or the soccer field, you might never even notice he has physical difficulties. If you have an idea in your mind of what Cerebral Palsy looks like, you’d probably never connect that mental picture with the boy in front of you.
Cerebral Palsy is a generic, blanket term doctors use for any damage that happens to the brain before about the age of two, and causes physical symptoms. Modern medicine now adds more descriptive words to CP to give a better indication of the exact presentation of symptoms.
My son’s CP was caused by a stroke around the time of birth, a common cause. The human brain is such a mystery to doctors, even today, that no one can tell from an MRI of an affected child just what their prognosis will be. One child might have a very small region of the brain affected (or nothing even visible on images), and yet be fairly severely affected. Others can have massive sections of the brain affected and have very mild symptoms. I say this to help give perspective if a child you are considering is noted as having Cerebral Palsy or abnormal brain scans.
When he first came home at almost seven years old, we concentrated on bonding and general health. My son’s symptoms are very mild, but he had NO stamina. We let him decompress, attach to us, run, play, and build coordination before embarking on a formal assessment of his needs (in our case this was approved and encouraged by our International Adoption Clinic). Depending on the severity of CP symptoms, neurology and therapy may be a more immediate focus for other children.
CP is probably a lot like other special needs – we’ve gone through a phase of “We’ve got this” followed by one of “Oh my gosh, there’s so much to research and address” at least three times in the two and a half years he’s been home.

Our first real foray into the CP world was a visit to a neurologist. We were given the option to do an MRI or not. Due to his age, all treatment would stem from his symptoms and not the results of an MRI, but we chose to have one to get a baseline image in case he even got a concussion playing sports. The MRI was also able to rule out a couple of rare structural causes for his original stroke, which is nice peace of mind.
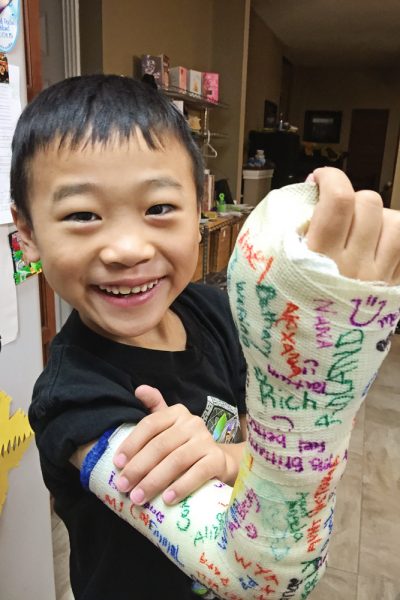
Our son’s main symptom is difficulty using his right hand. We saw the hand clinic at Scottish Rite hospital, and he underwent a tendon transfer and related orthopedic surgery after about a year home. They took the tendon he had the most control over and re-attached it in the location that would give him the most useful function when moving his hand. It was a very difficult recovery, since our very active 1st grader was not allowed to run, play, or sweat for five weeks (and in Texas, not sweating is hard even in the spring!). After the cast was removed, it was immediately clear that the surgery had produced wonderful results for our son. Weekly Occupational Therapy has allowed him to capitalize on the progress and make continuing additional gains.
Physical therapy was started to keep his affected leg as strong and flexible as possible. Growth spurts often cause increased spasticity in kids with CP, and the six inches he grew in the first two years home challenged us to keep up with ensuring he can run and walk smoothly! He is now also in an AFO (Ankle Foot Orthotic) to help get his toes up and out of his way as he moves, which has reduced his tripping tremendously.
After two and a half years home, my son is on a recreational soccer team, loves most sports, is close to riding a bicycle without training wheels, and is working at grade level in school. We are amazed every day at the ways he figures out how to work with the limitations of his body. We are just beginning to puzzle out some possible learning or processing differences, and are unsure if they are the product of hyper-vigilance, being in an SWI for almost seven years, or related to his stroke.

With most of his physical needs addressed, we are more confident entering this new phase. We’ve incorporated our son’s physical needs into our lifestyle, so it barely even occurs to us that not everyone’s kids do stretching exercises on weekday mornings. The OT is a part of our routine as well, just one of those after school activities we attend. Our days are filled with homework, soccer, Nerf guns, and fart jokes – typical nine year old stuff.
If you are considering a child with cerebral palsy, here are a few things to consider:
1. Medical science is just starting to really understand how much potential the human brain has to rewire around damaged area. Neuroplasticity is proven, and incredible gains can be made all the way through puberty, however many doctors, and even neurologists, have not kept up with this research. Do not settle for medical professionals who accept the status quo of your child’s functionality! Dr. Karen Pape has a fantastic blog that discusses advances in understanding of neuroplasticity.
2. There are amazingly supportive groups out there. Find them, and use the group’s combined wisdom to ensure you are getting the best care for your child. Yes, you and your doctor need to sift through the options and decide on the best course for your individual child, but collective knowledge can help you understand the jargon and know what questions to ask to find the best care possible.
3. Find a great neurologist that specializes in Cerebral Palsy. You’ll benefit from the knowledge of cutting edge research and therapy techniques. Our neurologist, even hosts conferences that bring together experts from all over America to share ideas and educate colleagues and parents!
4. The damage that causes Cerebral Palsy can also cause seizures. If you are reviewing a child’s file, be on the lookout for indications of seizures and educate yourself on the different varieties of seizure activity – some types do not resemble the classic grand mal seizures that are most often portrayed on TV.
5. Cerebral Palsy is caused by damage to the brain. Damage to the brain can also cause learning disabilities, some types of hearing loss, and some types of peripheral vision issues. I don’t say this to discourage families from considering this need, but to be realistic about the range of related issues that weren’t always acknowledged as part of CP in the past.
6. Just because you have a two-story house or other physically challenging situation, you may not need to rule out CP or other movement disorders. Many needs can exist on a continuum, and our son has no trouble navigating stairs or uneven terrain!
We began our adoption knowing our son had a medical need. This meant that we embraced his needs as part of who he was from the beginning – part and parcel with his smile and personality. I feel this has allowed us to cheer his accomplishments, enthusiastically research the best treatments, and embrace his therapies and equipment as exciting additions in helping him reach his potential.
We just live our particular life to the fullest.
– guest post by Bethany

























Another excellent post. Thank you! Our son has CP and we (and his OT’s) love seeing his determination in trying to gain strength in his weaker hand.
Thank you for sharing your story! We have only been home 3 months with our 4 year old who also has right side hemiparasis. Your story is very helpful as we begin to navigate through all of the challenges and glory. His biggest challenge is the hand, so perhaps seeing a hand specialist might be helpful! Thank you and blessings!
This was very helpful! Little guy we are adopting this summer has very similar medical paperwork, though not officially diagnosed with CP (we suspected early on so we are anticipating this diagnosis once we return to the states). I appreciate the info!