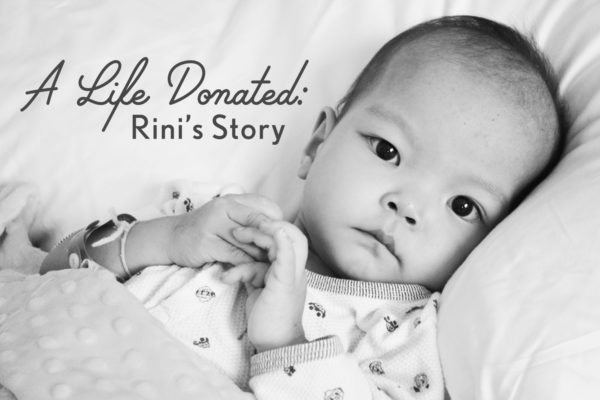
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
I have been giving a great deal of thought about what I hope to achieve with this series, as I did when I wrote a retrospective on Facebook for my daughter’s three year transplant anniversary. My biggest goal is to contribute to organ and tissue donation advocacy. Perhaps by sharing what it was like to watch our child move closer to death with each passing day, to beg for just one more hour with her and knowing that we would only be granted that by the choice of another family during their darkest time, it will illustrate to people the power of donating life. But also, I hope for healing for myself, and also to offer hope to families walking with their own children along paths that seem impossible to navigate at times.
More and more children are being adopted from China with medical conditions that will ultimately result in the need for organ transplant, and so many others will have a better quality of life, or better surgical outcomes, through tissue donation.
For this first post, after a brief introduction for those not familiar with my daughter Rini’s story, I will simply share portions of my journal and blog entries from this time almost four years ago.
I always welcome any questions that any of you may have because I remember that when I was new to the world of adopting children with Congenital Heart Disease, I often read posts and blogs and yearned to understand more about the nuances and management of CHD. Please feel free to email me if there is something you’d like to better understand. Becoming the parent of a CHD warrior is not for the faint of heart. These children need strong parents to support them in their battles and if I can be of service in any way, please let me know.
The Beginning

Rini had arrived home from China on August 29th after an expedited adoption of only three and a half months followed by our tumultuous trip. Hers was one of only a handful of adoptions to be blocked in-country in the history of the program.
We arrived in China to find her in a PICU nearing end-stage heart failure and in kidney and renal failure. Our steadfast and dedicated agency never left our side, and after their incredible work and diplomacy, we were at last permitted to adopt her. Upon landing in Oregon my husband had taken us straight to local children’s hospital where our pediatric cardiology team was waiting and we were admitted. She spent two weeks in the ICU where, after her full cardiac workup, cardiac catheterization and consultations with other hospitals, she was declared inoperable due to critical, severe malnutrition and end stage heart disease.
From a metabolic standpoint, her team surmised that she was within 3-4 weeks of death at the time we adopted her. As misguided as hindsight would later illustrate, we had been encouraged to take Rini home with the hope that she would gain strength within the love of our home, be enterally fed and allowed to blossom as our other children had done. It was not to be. This was my first indoctrination to the difference in experience and recommendation between a hospital lacking heart failure services and one with.
Nine days later on September 20th, 2013, she went into respiratory failure in the early morning hours and I rushed her to the hospital while Eric left work to come home to be with our other five children.
From my blog and journal – September 21, 2013:
“This is an extremely difficult post to write, and I’ve hesitated all day to give voice on this blog to what has transpired. I do not know if I will continue to post much publicly in the upcoming weeks and months. But I do want to update all of you at this point, and I hope that you will continue to pray for her strength and for our family to be able to accept with grace wherever her course takes us.
The duality of emotions is difficult to articulate. There is great pain existing in conjunction with great joy and peace…joy and peace that comes from knowing that we followed where led and have been given an indescribable gift by Rini’s presence in our lives.
I have tried to dance around this fact, but Rini’s heart is failing and she is dying. Our team came in yesterday and we discussed many things, namely the attempt to keep her out of the ICU for as long as possible. We all agree that we want to keep her in a less chaotic environment for as long as possible. Although admitting her to the ICU and supporting her with the big gun cardiac supports is obviously an option, we are weighing many factors. Every intervention has its consequences, and under the recommendation of more experienced centers, our team does not want to use up what few interventions exist until there is no other choice.
Eric and I opted to have her admitted to the Intermediate Care floor while they have added another cardiac medication (which was started on Friday) and increased respiratory support while monitoring the outcome.
Rini has not gained any weight over the past month, even on continual enteral feeding. Everything, it seems, has that domino effect. Today we began increasing her feeds and monitoring her body’s reaction to the increased volume. We have to be careful not to go up too much or too quickly, or she begins to throw up her feeds. We discussed changing her to a more calorie-dense formula, but when that was previously tried the change in fluid volume affected her cardiac function and it goes around and around. So as it stands, we have increased her feeds to give her an additional 300 calories per day and we are hoping to see some weight gain. Her labored respiration and cardiac function are consuming so many calories. This is a struggle for many children with heart disease, but exacerbated by the fact that she is so significantly malnourished already.
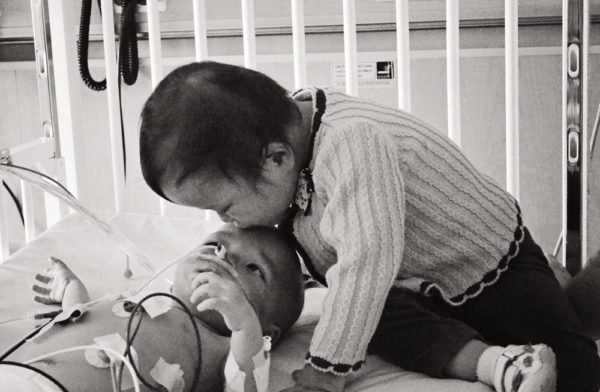
Yesterday evening two of our cardiologists came into her room and asked me what Eric and I feel is in her best interest. I told them that we understand what we are struggling against, that she can’t be “fixed”. I told them about our nine days at home, how she laughed and smiled, ate apple sauce, yogurt, and had her first taste of chocolate/vanilla swirl from Dairy Queen, how I took her with me each day to pick MeiLi up from school and how she pointed to everything and made her little “humf” noise to indicate that she wanted to know the name of the object, how she loved to be taken outside for walks by Sophie, loved her bath time, and held my hand almost all night through the slats of her little crib. We don’t want her life to be one continuous hospitalization. We want there to be a balance. We accept that keeping her here will not result in her getting better. Her hospitalizations are to find the line where her body is being supported. We hope and strive for stability so that she can come home and enjoy life while she hopefully makes some gains physically.
Today, I conferenced with several members of our cardiology team. They were very frank and honest which I appreciated. They have not seen any noticeable improvement with the introduction of the Digoxin, and her respiratory distress, which improved when she was placed on high flow in the ER upon her initial hospitalization, has slowly become worse again even though the high flow has continued. She is declining and it is looking like she may not be able to hold out for the weight gain that we all had hoped would bring some strength to her heart and also give her the metabolic boost necessary for surgery.
Judging by her echocardiogram, they and the teams at the other hospitals they consulted with are in agreement that her heart would not be able to withstand the job of pumping after her tricuspid and mitral valves are repaired/replaced, which would be the first in a line of surgeries necessary to prepare her for the Glenn/Fontan palliations. She is too malnourished to undergo surgery right now anyway. She is struggling enough to heal from the minor wounds she came home from China with, such as a burn from having had a pulse oximeter left on her toe for too long in the PICU in China five weeks ago.
So where it stands is that Eric and I will begin working with our team this week to start the process of evaluation for heart transplant. I found myself avoiding contacting our insurer and discussing transplant benefits, probably out of a sense of denial, but I finally forced myself to do so last week and we are now in the process of researching the centers that we may choose from. Her transplant benefits are in full effect, which is a huge relief.
Our doctors also discussed with me our other option, which is to choose compassionate/palliative care and come under the care of Bridges, which is our hospital’s pediatric hospice organization. Just hearing those words spoken out loud, although Eric and I have both gone down that road in our minds, was utterly painful.
I don’t think that there are words in existence to adequately articulate how this feels. We are still hoping that we will be surprised by a turnaround in her cardiac function coupled with muscle gain that will permit at least the first needed surgery to be an option, but we also see the reality of the situation and we feel that we need to act within the window that she has.
Of course our biggest fear is that whatever choice we make for her will cause her more harm than good. And I am grateful for our physicians who admit that there is absolutely no way to predict how a child in Rini’s position will respond to whatever intervention is attempted. I stare at her and I am devastated when I imagine that she might not have the opportunity to grow up and enjoy the act of living. Will we ever hear her little voice speaking to us? Will we ever see her walk? All of these little things that we usually take for granted have taken on a new urgency to us now.
I remember having a conversation with a friend who has several children with complex heart disease. She expressed her fear that as they adopted each subsequent child, their luck would run out. I remember that conversation so vividly, as I have wondered the same thing. We have had such great outcomes with Tristan, Bryce, and Scarlett. Yes, they all need additional surgeries. Yes, Scarlett has hypoplastic left heart syndrome with all that comes with that diagnosis. Yes, she and Bryce had difficult recoveries from their surgeries with several frightening setbacks during the post-op period. But today I kept hearing that conversation in my mind.
And I also remember thinking how each child’s adoption and medical needs prepared us for the next, and here we are. But that realization also brings me strength and peace, because I see the path that was laid out, and I know we are not alone in this. There is a purpose.
Rini is a beautiful child, with a gentle spirit. But surprisingly, she has a really loud voice when she wants to use it! She seems to prefer to use it multiple times during the night to let me know that she needs her diaper changed or that she has lost her grip on my finger! She loves to look at books, claps for herself after her blood draws, and likes to listen to music. She thinks her siblings are hysterically funny, she doesn’t like cats, and she loves yogurt. Her eyes are gorgeous, she makes you really earn a smile, and she sucks her thumb at night.
Choosing to let her into our lives and into our hearts is one of the best decisions that Eric and I have ever made.
When you love a child, you are making the choice to allow someone else to walk around with your heart in his or her hands. And we have found that when you love a child who has the potential to break your heart, those little cracks open your heart up bit by bit until you realize that you now have the capacity to love more fully than you ever thought possible, and to love more children than you ever dreamed of.”


























I’m holding my breath for Part 2 of this blog! I check almost daily to see if it has appeared.
Thank you for reading our story, Emily!