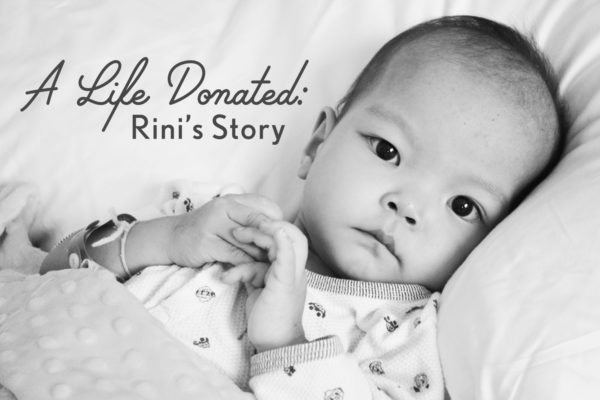
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From my journal – September 22, 2016:
Impatience has no place in your life when you’re walking with your child down an uncertain road. You cannot force an answer to the question of whether your child will live or die. Not from man, not from God. You have to learn to accept silence. You have to learn to embrace the fact that there may be no answers, that medicine is as much art as it is science, and that there is no handbook for these complex children. And as you learn to wait, you must learn to still live during that time and to find the joy in every day, even the darkest ones.
This day three years ago was when the colossal load of waiting began to seep into our consciousness. It already felt heavy, but we had absolutely no conception of how precious and sacred every minute would become in the upcoming weeks, and how desperately complex the process of waiting would be.
It was the beginning of our receiving what we have come to call “Rini’s Gifts”.

It is surreal reading my journal from 2013 with the benefit of hindsight. What strikes me is how with each passing day, the belief that we were holding the reins in any way, shape, or form slipped further away. That liberation from the false sense in control is another one of Rini’s Gifts.
From my journal – September 22, 2013:
“Today Rini’s materials were sent to the transplant center at Stanford to begin the process of evaluation for transplant. We have been advised that she may need a heart/lung transplant rather than just heart. We also know that she may not be found to be a good candidate for transplant. If she is and we make the decision to list her, there is no guarantee that she will be a recipient. But we are hoping for positive news that we can work with.
There is a book by Art Spiegelman entitled Maus. In it, the author tells the story of his parents and of their experiences during the Holocaust and surviving Auschwitz. In one part of the book, the author goes to his therapist and they have a discussion about survival. The author comments that his father was very resourceful to have survived the camp, and his therapist responds by asking if he admires his father for surviving, to which he answers in the affirmative. His therapist then says something that has been going through my mind over and over for the past few days.
“So it’s as though life equals winning, and death equals losing, and the victims are then to blame. But the best didn’t live and the worst didn’t die. It was random.”
Life equals winning and death equals losing. I feel that many people view it that way. And I know that Eric and I are struggling with what constitutes success in Rini’s life, and the feeling that if we can’t make this turn out well for her, we have failed.
Rini’s heart function has shown no improvement, and she cannot manage without respiratory support. Because high flow is not available in the home setting, within the next day or two she will be moved to the PICU and she will be assessed with CPAP support. Our hope is that it will provide her body with enough relief during the night that she can be free of it during the day and enjoy a bit of normalcy. Or, she may need it 24 hours per day.
Given that she is nearly at end stage cardiac disease, there is a real concern that she will not be able to survive long enough for transplant. If she is a candidate and we list her, she will most likely need to be hospitalized at the transplant center with intensifying cardiac and pulmonary support.
As answers come in from Stanford and other centers, we will be making our decisions. We have been the beneficiaries of incredible support and love by everyone involved in her care. The past two days have been especially difficult, as almost every conversation turns to making end of life decisions for our little girl. Tomorrow, the hospice team will be meeting with me, and today I spoke with our beloved Holt social worker that has been through all of our adoptions with us over the past 8 years. She is providing guidance as to how to best support our other children during this time and, in particular, if Rini enters end of life care at home.
One of the Child Life specialists came and sat with me today as Rini slept, and she said that there is an ethics committee at the hospital that we are welcome to meet with, as Eric and I are struggling with myriad emotions, including guilt and doubt. How do we decide for another human being? What is the right thing to do for our child? How do we know when it is time to let go? Which decision is merciful?
Today I spent talking with the wound care department about managing the care of Rini’s body, namely her nostrils and nose, since she will have her NG tube in indefinitely. We briefly discussed having a g-tube placed for her enteral feeding so that she won’t have to have the discomfort of the ng-tube, but all parties involved gave an adamant “no”. First off, sedation is too risky for her plus her diaphragm is already so compressed because of her severely enlarged heart that they wouldn’t be able to perform the necessary dilation of her diaphragm during the g-tube placement without compression of her heart and lungs. Before she goes on CPAP, she will have her swallow study to make absolutely sure that there are no anatomical anomalies in her throat which would cause aspiration as we work towards beginning oral feeds again. They have not been allowing them since her re-hospitalization since they’ve been working to increase her NG feeds, and she is tolerating the increase well. So as long as she has no aspiration issues, we will be able to re-introduce her favorite foods soon.
Pulmonology is currently assessing her respiratory situation and either today or tomorrow she will be moved into the PICU and will be placed on CPAP. The goal is to see if it helps to bring her out of respiratory distress and assists her cardiac function by removing some of the labor of breathing. What we are hoping for is to be able to take her home on CPAP. She can’t manage outside the hospital without the respiratory support so that is our hope of being able to go home for a time.
One of the most beautiful and painful processes that is taking place here is watching Rini’s spirit come alive as her body fails. She is absolutely stunning in her beauty and her spirit. Everyone adores her. I have woken up to the sounds of nurses and doctors singing softly to her and cooing at her. And I’ve seen several of them well up with tears as they look at her. We are so, so blessed to have a hospital where we are treated like family. And because the adoption community is tightly knit and there are many families whose children with CHD are treated here, everyone knows everyone and it creates a feeling of warmth and support.
On Sunday morning, one of my closest friends died after a life long battle with Cystic Fibrosis and, more recently, cancer. Only minutes after learning of her death, Rini called me “mama” for the first time. Now she commands me around with her surprisingly loud voice, “MAMA! MAMA!” as she points to something she wants. I think she is enjoying having someone caring just for her for the first time in her life. She loves to be bathed, to have lotion rubbed into her skin, to be hugged, and held.
Last night her nurse and I were chatting across the crib from one another. Rini yelled, “MAMA!” and we looked down. She had managed to balance an empty syringe between her feet. I didn’t get the photo right at that moment, but did take one as she was attempting to replicate her feat. Just look at the determination on her face!”

From my journal – September 24, 2016:
Three years ago today, we were very anxiously waiting to hear if the transplant centers that Rini’s team was consulting with would deem her a candidate. Not a candidate for transplant mind you, but first a candidate for transplant evaluation. Just when I thought I couldn’t get any more nervous, another layer would be peeled away and I’d be thrust into a realm of uncertainty unlike anything I had ever experienced. Little did I know how much harder it would become. We still thought we had time. But in only 17 days, Rini would begin her very rapid decline into end stage heart failure.
Time would become an obsession.
I was struck early on in our lives with how Rini accepted the cards she had been dealt. I’m not referring to the surrender that many children (including some of my own) with chronic illness exhibit after they have been beaten down by too many painful procedures. But rather, Rini has always seemed to accept that it is what it is, and she proceeds with grace. Grace.
Oh how this child has taught me to strive to live with grace!
After they were finished drawing her blood, Rini would blow kisses to the phlebotomists who came in once or sometimes twice per day, and she waved and smiled at her caregivers even after they had intervened in a painful way. She forgave, and continues to to this very day. And she always found a way to be involved in her care and to have fun in the moment during those weeks and months.
She was a testament to the power of living even as she was dying.


























Very beautifully written. Is there are part 3 to this coming up?
Lina, thank you for reading! NHBO has graciously committed to posting installments of this series for the next several months.