Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From October 11th, 2016
On this day three years ago, I was packing for the following day’s trip back to the hospital. I was so excited to see my beautiful girl again, and so consumed with guilt for having to leave our other children.
Our friends had referred us to a photographer who had generously offered to come to the hospital in two days to take our family portrait. The thought of Rini dying and not having been in a photograph with our family was an insult to my heart and soul.
In my luggage, I had carefully placed the dress, shoes, and headband that I had chosen. Oh how I had obsessed over that outfit! All of the seemingly mundane tasks that we take for granted in our day-to-day parenting – preparing a meal for our children, bathing them, selecting their clothes – are so very precious.
I feel fortunate that I understand and appreciate that now more than ever.

We began looking forward to taking Rini out of the confines of her hospital room after her doctors had given their consent for us to go to different areas of the hospital, including an outdoor patio, for the session. But that plan would change.
In just 48 hours, Rini’s heart would enter its twilight and begin communicating to us just how tired it was.
From October 12th, 2016
“Trust in the Lord with all your heart and lean not on your own understanding.”
On this day three years ago, Eric, our children and my parents drove up to the hospital for our family portrait session. What a mixture of hope, sadness, beauty, and grief that day was.
Early that rainy Saturday morning, Rini’s cardiology team and nurses told us that they were not going to permit her to leave her room after all, even on respiratory support and with nursing care. That’s all they said. Looking back on so many interactions with our teams, both in Portland and later at Seattle, I can now clearly hear the words that were not spoken.
The photographers set up and for the next twenty minutes we sat together as a family and captured precious moments. It was a joyful time, with the kids playfully interacting, smiling a lot, and enjoying themselves.
It was another of those times where I felt like God was giving us a big hug. I was so grateful to experience that togetherness without the typical stress and sibling squabbling that seemed to always be a part of family portrait days of years past.

The only child who was not smiling that day was Rini, and I remember that sick, sinking feeling in the pit of my stomach masked by my smile. I knew something had changed and after the first twenty minutes, it became clear to all of us that Rini was struggling.
We put her on her bed and reattached her pulse oximeter and telemetry, and saw that her 02 saturation was dropping and she was tachycardic. Her nurse was able to stabilize her after some time, and the cardiologist was paged.
In just 72 hours, we would have our first conversation ever regarding our resuscitation wishes for our child.
From October 14th, 2016
On this day three years ago, Dr. Carlson came into Rini’s room in the late morning and handed me a notebook that would change everything. The cover read, “Living With a Heart Transplant” and it was from Seattle Children’s Hospital.
Did that mean they had accepted her for transplant evaluation?!
I remember feeling like I was in a state of suspended animation. Time seemed to stand still.
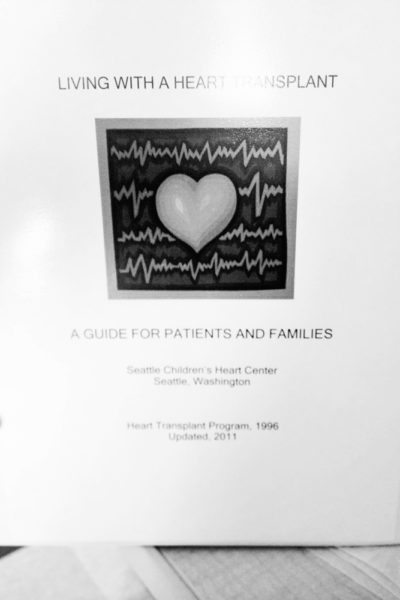
Seattle had notified Rini’s team that they would accept her for evaluation if her prealbumin reached 18 mg/dL, and the hope was that she would be in a position to transfer there on the 23rd. They wanted us to read through the book to gain a thorough understanding of the process of evaluation, listing, transplant and its lifelong aftercare, in order to make a determination as to whether this course was truly what we wished to pursue for Rini.
As would be reiterated to us more times that we could count, transplant is not a cure. It is “trading one chronic condition for another”. Its goal is to extend life and improve its quality.
It is a gift.
It is a responsibility.
Some families ultimately decide against it for their child for various reasons. But for us it was the only offering we could make to her. Hope was the only gift we could bestow upon our child. We couldn’t see any other way than to continue on the path we were on, to try for her sake, to endure, to trust in God that there was a reason for it all.
To this day we are grateful to all of the physicians and other medical professionals involved in Rini’s care for supplying us with unbiased information and not burdening us with negativity or unsolicited opinions.
Eric and I did our research. We understood the odds. And not for one minute were we unaware of the responsibility of that choice, despite what some might have thought. It’s easy to take the moral high ground and declare, “I would never!” when you are parenting healthy children.
In an unbroken world, no parent would ever be put in the position to have to choose between witnessing their child suffer and die or watching their child suffer in a battle for their life. Opinions rooted in concrete are often the privilege of those on the sidelines.
I was cautiously optimistic, yet at the same time in a state of panic. Rini wasn’t metabolically stable yet, and her declining state had thrown her body into the beginning stages of chaos.
Yes, she was already in chaos. But I have to be very careful with the words I choose and the way in which I quantify, as we would soon learn how many layers there are to “sick” and to “dying”. I had absolutely no appreciation of that at the time.
A friend came to visit Rini and me the very next day and she said, “I thought she would look different, like with tubes all over.” That same friend would visit us a few weeks later in Seattle, when Rini was on life support, intubated and with ECMO cannulas bringing her entire body’s volume of blood out of her and back in, in a relentless dance of agony and hope. There is dying, and then there is dying.
Rini had been gaining a few grams per day, but was now having diarrhea along with vomiting. Labs were being checked every morning at 5am, and sometimes twice per day. We learned that Seattle was now steering the ship and guiding Rini’s team on her care, and all new support would need to be approved in order to make sure that nothing was done that could adversely affect her transplant eligibility.
For instance, some of the cardiologists had suggested occluding Rini’s PDA (patent ductus arteriosis) in the cath lab within the next day or two in order to increase her oxygen saturation but Seattle vetoed that. In the blur of all that was happening, I didn’t understand why but the reason would be made very clear on November 7th, and would open our eyes to just how vital it was to have an experienced heart failure/transplant team in charge of a child like her.
Although Dr. Carlson had sat down with us a couple of weeks prior and walked us through the physiological process of death by heart failure, watching this disease assault our child was something we could never have prepared ourselves for. Neither was being in a situation where our daughter’s chance at life would hinge on the decisions made by strangers.
We would be taken down a path where our struggle for control would be beaten out of us day by day, and as agonizing as it would be, it was for our own good.
“Three times I pleaded with the Lord about this, that it should leave me. But he said to me, “My grace is sufficient for you, for my power is made perfect in weakness.” Therefore I will boast all the more gladly of my weaknesses, so that the power of Christ may rest upon me.” 2 Corinthians 12:8-9



























Leave a Reply