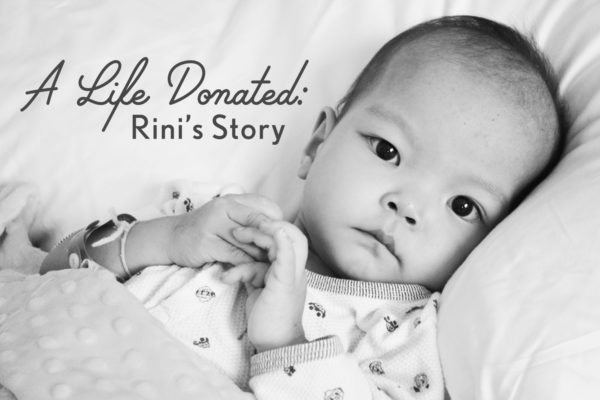
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From November 8th, 2016
On this day three years ago, Rini continued to struggle on ECMO. I woke up to see several of Rini’s cardiologists talking with the ECMO perfusionists. I caught bits and pieces of the conversation and a while later, a portable CT scanner arrived in the room. Not much was said about why it was there, and I didn’t ask many questions. They probably chose the “less is more” road in order to decrease the possibility of having a hysterical parent on their hands, and I chose not to press because I already knew why it was there.
Her paralytic medication had been lifted hours before in an attempt to gauge her neurological condition, and she was not responding to stimuli. They were concerned that she had suffered a brain hemorrhage or was experiencing swelling.

From my journal:
“A bit later they rolled in the bedside CT machine, the same one that I saw going into the room of the little girl that passed away while on ECMO the night that we were told they would be listing Rini for transplant. The scan took about fifteen minutes, and of course the technicians wouldn’t tell me anything. I kept trying to read their faces but it was useless. I asked how long until the radiologists and neurologists would read the scan and get back to me, and she said in about fifteen minutes.
After two hours, I asked the nurse to check on the status of the report, and an hour later one of the other ECMO specialists came in and didn’t see me sitting in the back of the room. He asked the others if they had seen the report yet, as he had. I jumped up and said, “I know you are going to tell me that you can’t tell me anything, but just help me out here.” He let me know that things looked good, but it was still another hour until one of Rini’s doctors came with the official report, which was: no sign of edema or bleeding, although they did see a small area that looks like a very old bleed. They also noticed areas of atrophy that they attribute to her prolonged malnutrition, and the neurologist said that damage such as that is usually reversible with time. We are not concerned. It’s the least of our worries. We are just so incredibly relieved that she is still with us. I went to my favorite alone spot – the bathroom down the hall – and cried.”
Last night while preparing for bed, Eric and I were talking about this retrospective and I commented that I feel that I am failing to articulate how it felt during those most critical of days. But I honestly don’t feel that there is a way for me to. There was the constant onslaught of adrenaline rushes; the sick, choking feeling; the fear; the pain; the anxiety. And through it all, the hope and the beauty residing right alongside.
One minute a doctor delivered bad news, the next his colleague broke out his iPhone to show me a funny video and I’d be laughing through my tears. And the hardest thing to deal with was the juxtaposition of life and death, of recipient and donor, of wanting the chance to celebrate my child’s saved life when at the same time, another family would be mourning their child’s death.

From my journal:
“And then just like that, we went from fear and pain to elation. We have been struck by how the line keeps getting pushed out further and further, and how things truly are relative. A month ago, “stable” meant a day that she was breathing a bit easier and keeping her feeds down. Three days ago, “stable” meant that she had gone 24 hours without another cardiac arrest. Today, “stable” means she is on life support and tolerating it well.”
During this time I obsessively checked the UNOS statistics on the website provided to those whose children are listed. I learned that there were a total of four children in Region 6 listed for cardiac transplant. One of those children was residing in the room right next door to Rini’s, and his mother and I became friends. Her toddler son spent almost every day at the hospital with her and I loved seeing him playing! It was such a joyful reminder that life goes on. His mom allowed me to take him on outings in the hospital on a few occasions which I loved. His baby brother had spent his entire eight months of life in the CICU after being born with Hypoplastic Left Heart Syndrome, and he received a donor’s heart just a couple of weeks after Rini. His hero heart gave him another four months of life before he left for Heaven. Eric and I talk about him so much, along with his beautiful family who was such an encouragement to us.
Because of the shortage of hearts, UNOS has allocation rules. For instance, time accrued on the waiting list is taken into consideration when the computer decides which patient an available heart will be offered to. However, because children on ECMO have a finite amount of time on life support, in July of 2015 UNOS changed their policy. Since then, a child at Status 1A who is on ECMO will automatically be placed ahead of a child at the same status even if that child has been on the waiting list longer. But when Rini was waiting, that rule was not in effect. To be worried about where my child would be on a list was such a horrible feeling, As much as I wanted Rini to have a chance at life, I didn’t want another child not to. It was terribly, terribly confusing and painful.
Another allocation rule has to do with blood type. Because some blood types are compatible with more blood types than others (for instance, those with AB blood can receive a heart from any blood type, whereas a patient with 0 blood can only receive a heart from another 0), UNOS developed a system in an attempt to make things more equitable. Because O is the “universal donor” (and most common blood type) and AB is the “universal recipient” (and rarest blood type), now an AB can receive a heart from an A, B, or AB (but not O) and an O will only go to an O or B. Rini has blood type A and can technically accept a heart from an A or O donor. But the allocation rules only allow an “A” to receive from an “A”, not from an “O”.
And although some children under the age of two may be able to receive a heart from any blood type because their immune systems are immature, Rini was not a candidate for this (even though she was listed when she was under 24 months of age), because of her high antibody counts. I spent many hours pouring over data, trying to ascertain Rini’s chances of being matched with a precious heart. And as I did so, I felt awful about it.
Of course I didn’t know it at the time, but many of the people I had developed relationships with during my kids’ time in hospitals, particularly Rini’s, would become knit together in a beautiful way and lead to the blossoming of the Little Hearts Medical team.
From my journal:
“After Rini was placed on ECMO yesterday, I was approached by a young cardiologist who asked if I would consent to Rini participating in a study investigating the effects of ECMO on thyroid function. I had no problem with that and we began chatting and he asked to hear our story. I love to tell about how we came to our children and he listened and at the end of it, he reached into his coat and wrote his email address on his card and said, “I will review any and all CHD files that you send to be as part of your advocacy work.” I was so grateful and excited! Our interventionist in Portland reviews files for me but to have two willing to help will be huge!”
That was the beginning of the file review service that was instigated when I took my position with LHM, and the doctor who approached me that day was Dr. Files, who alone has performed the reviews of a huge number of the files LHM has received over the past three years, thus helping so many CHD children from China come home to families.
From November 9th, 2016:
Three years ago, Rini’s day was relatively uneventful. Relatively. It was another word whose meaning was fluid in our world, right along with our ever-changing definition of stable. Her ECMO circuit had to be changed again because of fibrous clots that had formed, but the procedure went without a hitch. The circuit was shut off and the change had to be performed as quickly as possible since she would not have any blood flow during the intervention.
From my journal:
“Her paralytic medication was lifted and twice today she began to move around and this morning she tried to open her eyes and she grasped my finger. After the ECMO circuit change, as her sedation was wearing off, she again began moving around and became quite agitated. I held her hand and talked to her and she settled, and for the first time in two weeks she opened her eyes about half way and looked at me. I was able to capture it on video to send to Eric and it was one of the most treasured moments of my life.”
She was not able to come out of sedation for very long before she began to experience alarming arrhythmias, which over the next 24 hours would begin to increase in frequency and severity even while fully sedated. That evening, I was pulled aside by one of the transplant cardiologists who informed me that because of Rini’s continually declining state, they had changed Rini’s listing with UNOS. She was still listed as able to receive a heart form a donor as small as 6 pounds, but the upper weight limit had been increased from 34 pounds to 65 pounds in order to “cast a wider net”. I remember listening to her in a state of disbelief. I couldn’t process what she was communicating to me. During those days, there was so much information relayed between the lines, and I was just beginning to learn how to decipher this medical language of my child dying.
November 10, 2013:
From my journal:
“On the days when Rini isn’t in perpetual crisis, I tend to have my most difficult moments as I have the time to think and feel all that is occurring. I am extremely agitated and I am so worried that a heart will not come to her in time. I have been hyper-analyzing the transplant data and started asking one of the transplant cardiologists a lot of questions about wait times, statistics, and the like. She was very compassionate and gently reminded me that pouring over the details is a moot point. I know she is right, and at that time I removed myself from the CICU and spent a couple of hours upstairs in the family center, reading and talking with friends.”
We received such compassionate support from friends and strangers alike during those days, but there were some who were not so kind. In response I wrote:
“Those who know us understand this about us. But for anyone who is wondering, we are very acutely and painfully aware that a heart for Rini is not magically growing in a laboratory somewhere. We do not need to be reminded that if she receives the gift of a new heart, it has come from the death of another person’s precious son or daughter. We have had a few people feel the need to tell us that, as though we are not already well aware of that fact. I hope that people can trust that anyone in our position recognizes the complexity of this situation. We do not pray for someone else’s child to die.”
……..






















In all the years I’ve read NHBO, AP blogs from Chinese adoptions and elsewhere, etc., I’ve been struck by the aplomb – among many other attributes – of adoptive parents who confront ignorant, critical comments from others – and that includes the ones coming from “a good place”. Yet today I gasped at my own naivete, for starters, wondering how self-righteousness and/or condescension could possibly be the modus operandi of any human in response to parents of a dying child.
Perhaps, instead of anger, I could pity those afflicted by savagery: there is no
cure for an absence of mercy – at least not a medical one.
This series is astonishing. Thank you for chronicling your travails for those who will come after. God bless you and Rini, especially. 🙂
♡♡☆☆
Thank you, Brett!