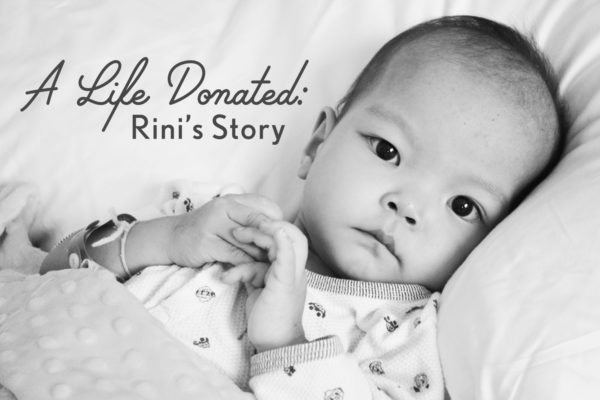
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From my journal – September 25, 2016:
“On this day three years ago, Rini was permitted to go on a short stroll around the unit. We began our outing with her in the stroller, but ended it with her in my arms. I wanted to feel her little body against mine. I still remember how she nestled her head into my neck. It was the sweetest thing. Looking back, I see those days as so easy, so peaceful, compared to what was to come. We were still waiting to hear back from the transplant centers, and we still felt like she had a relative abundance of time. Rini, with her fighting spirit and matter-of-fact attitude, tricked many of us.”
From my journal – September 26, 2016:
“On this day three years ago, I was enjoying having my baby girl in my arms. She was so playful that afternoon and I was hopeful that she was gaining some ground. We were still waiting on the decisions from the transplant centers regarding evaluation candidacy. At that point, we thought the main hurdle we needed to cross was getting her accepted for evaluation. It hadn’t sunk in yet that she might be accepted for evaluation but then denied for transplant listing. The reality of that possibility would come soon enough.”

From my journal – September 27, 2016:
“Three years ago today, I began experiencing a cluster of physical symptoms that would occur more and more often over the upcoming weeks until they became my constant companions: cold, clammy skin, lightheadedness, elevated heart rate, butterflies in my stomach, a dry mouth, shaking hands and tear-filled eyes. Anxiety, near panic, desperation, and ultimately, crushing sadness that would become almost overwhelming.
It was on this day that the transplant centers our team had contacted said “no” to Rini for transplant evaluation. Seattle still had not weighed in yet, but there was no reason for us to believe that they would feel any differently. And, as it turned out, they didn’t, at least not at first.
On this day, three years ago, we were told that Rini was far too metabolically unstable and malnourished for transplant, and her anatomical complexity also made her a very high risk. “Re-approach us in several months,” was the answer, “when she has put on weight and her metabolic status has improved.”
There were a few members of the cardiology team at our home hospital who felt that Rini would survive for several more months, but not all. Her primary cardiologist didn’t. Her interventionist didn’t. The surgeon didn’t. The ICU cardiac intensivist didn’t. Neither did we.
And Rini herself would show us in just a few short weeks that she wouldn’t.
A few days later, as a group of cardiologists who had never examined Rini prior to that morning were in her room for rounds, one of them began arguing this point with me:
“The transplant centers didn’t really say ‘no’,” he retorted at me, “they just said, ‘not right now’.”
For the first time in my life, I took a deep breath and got a little mouthy with one of the white coats.
“Really? Are you honestly going to stand there and try to convince yourself and me that she has several more months of life in her?”
I was met with silence.
“From now on, I only want to discuss Rini’s case with her primary cardiologist.”
This was the beginning of our separation from the hospital we loved, a center that had taken such good care of our family for three years. Not a separation stemming from anger or betrayal, but one coming from a slow progression rooted in a stark realization. Rini needed a center with a program devoted to and experienced with other children just like her, children whose remaining heartbeats were few. We needed a heart failure program. We needed a transplant program. And we prayed that one would open their hearts to her.
Three years ago today was also the day that we met with our hospital’s hospice program.”
From my journal – September 27, 2013:
“This past week has been so emotionally taxing, that today I could barely muster any emotions. I am so eager to get Rini home, but also keenly aware of the complexity of what is to come. The head of the hospice program came to meet with me and she was absolutely amazing. She stayed and spoke with me for about an hour, outlining the support services available to Eric and me, Rini, and our other children. She also explained how, if we choose, we will be partnered with our local hospice organization to help us to care for Rini and to guide and support our family as we help Rini transition from this life. They provide art therapy, music therapy, and bereavement counseling to siblings, have musicians who will come to the home to provide music for the child, and of course, provide medical personnel to teach us how to control Rini’s pain and make her days as comfortable as possible.
And the most important thing she told us was that it is perfectly okay to plan and prepare for a child’s passage from this life while still hoping for physical healing. Especially with other children involved, we cannot afford not to educate ourselves and work towards providing for the emotional needs of our entire family.
We also reached out to Holt and our Holt social worker who has been with us through all of our adoptions for their guidance in how to best handle this situation in view of the fact that our adopted children have histories that need to be taken into consideration when deciding how best to support them in the death of a sibling. We also need to be sensitive to the fact that we have three other children with cardiac disease who have continual medical needs and will have future interventions and surgeries. Helping them to process Rini’s situation in light of their own health concerns is something else we will need to focus on.”
That was also the day that Rini had a barium swallow study that showed severe silent aspiration of both thin and thick liquids and foods, meaning that her oral feeds would have to be ceased immediately. My daily ritual of spoon-feeding my baby delicious pudding, ice creams, and yogurts in an attempt to bring some diversion and joy to the long days in her crib had to end.
It began to feel like the walls were closing in little by little, and the reality that my child was in the process of dying was becoming increasingly clear.

“On this day, three years ago, nurses and physicians and other support personnel were coming and going into the night. At last it was quiet and Rini was asleep. I went to the laundry room to gather the blankets I had put in the wash that morning but had been unable to retrieve earlier. And like salt in my wounds, I saw all of her blankets folded neatly by a kindhearted parent and placed on top of the dryer except for the quilt I had made for her by hand. The quilt I had wrapped her in on the day she had become our daughter in China had been stolen. And at that point, there in the laundry room, I cried all the tears that I had been gathering up throughout that day and week.
Losing the blanket that I had poured my heart into with every stitch… lovingly choosing the fabrics, washing, drying, pressing, cutting, assembling… has now become a symbol of the losses to come. In particular, the devastating loss that would be experienced by a family I have never met, a violent severing from them of everything they held dear. I lost the blanket that I had wrapped my baby in. But they would lose their baby. And then they would choose to share their child’s earthly body so that others might live, so that my baby might live.
The immensely intense dance of emotions, of choice, and of fate would soon begin.”
From my journal – September 28, 2016:
“Three years ago today was the day after the worst day yet. Eric and I always attempted to remain mindful that it could always be worse. At least Rini was still alive, and at least there was still a glimmer of hope. Keeping that perspective and doing our best to keep our rose-colored glasses firmly on our faces aided us tremendously in remaining strong and upbeat for Rini and our other children. It would become increasingly difficult, however.
At this point in her hospitalization, each day consisted of different doctors and respiratory specialists tinkering with her 02 and high flow, weaning a little of this, adding a little of that. Everyone was still focused on trying to find that sweet spot of support that would enable Rini to come home while we waited and hoped for an improvement.
Eric was making phone calls to medical equipment companies across the U.S. trying to find a way to bring high flow to our home so that Rini could be supported there. Cpap was a disaster for her, and supplementary 02 accelerated her heart failure. It was high flow room air she needed to support her one functioning lung and take some of the burden off of her massive, diseased heart that had completely crushed her gravely underdeveloped left lung and pulmonary artery.
My mother’s instinct was telling me that it was not to be. I didn’t think Rini was going to make it home, and I wasn’t convinced anymore at that point that home was even the best place for her.”



























Leave a Reply