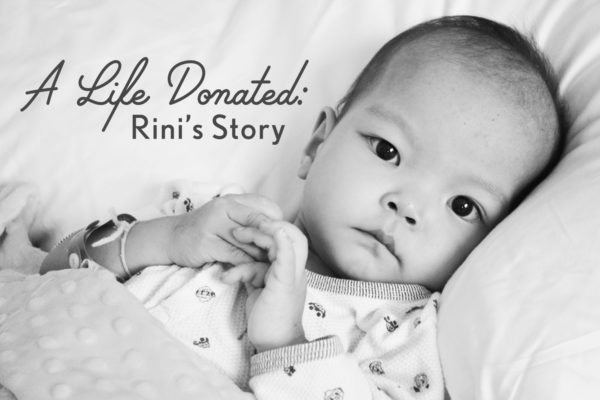
Rini, our youngest of six children, was adopted in August of 2013 at end stage heart failure stemming from complex, single ventricle congenital heart disease. She was admitted to the hospital immediately upon arrival home and within two weeks it was determined that she was inoperable, her only hope would come through cardiac transplant. She was initially found to be ineligible, but that would change thanks to a heart failure/transplant program that chose to take a chance on hope and optimism.
Much as we owe her life to the sacrifice made by her birth family in letting her go, we also owe it to the incredible, selfless act of organ donation made by a family in the midst of the incomprehensible loss of their child.
This series is a retrospective of the weeks leading up to Rini’s transplant which took place on November 13, 2013, and it is my hope that it will help to bring awareness to the importance of registering to be an organ and tissue donor.
We all have the power to be someone else’s miracle.
Donate Life!
From October 28th, 2016
On this day three years ago, Eric sent me this photo taken from Rini’s room. Many times I rejoiced that she was in a hospital so beautifully situated, as we could look out any window and see God’s glorious creation. It brought moments of peace during those days of great emotional chaos.

From October 29th, 2016
On this day three years ago, Seattle’s transplant surgeons approached Eric and told him that they had ordered a VAD (ventricular assist device) from New York for Rini. At the time, the details were a blur but yesterday I emailed the transplant team for clarification. Earlier this evening I received a phone call from Dr. M, Rini’s transplant surgeon. He was gracious enough to give of his time to discuss with me the parts of Rini’s story that I needed clarification on.
Ventricular assist devices can be used as a bridge to transplant and can be an alternative to ECMO (extracorporeal membranous oxygenation). ECMO is basically bedside cardio-pulmonary bypass, and takes over the function of the heart and lungs. The ECMO circuit moves blood out of the child’s body, through an oxygenator, and then back in. It is sometimes used to give a struggling heart the chance to rest after open-heart surgery but in Rini’s case, it would be an end-stage intervention. For her, it would be life-support. Outcomes in such cases are usually poor, since a heart like Rini’s does not recover and therefore the ECMO course would be indefinite. Massive doses of Heparin are used in an attempt to keep the ECMO circuit from clotting, and with the anticoagulant comes a significant bleeding risk. Another great risk is that of clotting, plus infection may occur and frequent blood transfusions are necessary. The longer a child is on ECMO, the greater the risk.
Placing Rini on ECMO was something that nobody wanted to do that early in her wait on the transplant list. With 3-5 months being the average wait for a heart in the U.S. at Status 1A, and with the average pediatric survival on ECMO just 2-3 weeks, well, the math was pretty ugly.
The VAD that was ordered was a PediMag, very similar to ECMO but without the oxygenator. Because of the absence of the oxygenator, less Heparin would be needed which would theoretically reduce the risk of a catastrophic bleed. VADs usually do not produce good outcomes in single ventricle patients, and depending on the child’s anatomical particulars, a VAD may not be an option at all. But because Rini had a PDA (patent ductus arteriosis), the hope was that enough blood would be able to make its way to her lungs for oxygenation in the absence of a mechanical oxygenator. It would not be a sure thing but with our consent, they wanted to try.
From her medical records:
“Rini has single ventricle CHD in the form of double inlet left ventricle, L-Transposition, severe subvalvar and valvar pulmonary stenosis, severely dilated right pulmonary artery, severely hypoplastic left pulmonary artery, severe right and left atrioventricular valve regurgitation, patent ductus arteriosis, severely dimished ventricular systolic function with severe left ventricular dilation.”
During this evening’s conversation, Dr. M said, “There were no good options for Rini.” But the hope was that the VAD would provide Rini with days or maybe a few weeks without the need for ECMO. Reflecting on those days, I see now what I didn’t understand enough to see then. Her team recognized where Rini’s journey was heading, and it was becoming a numbers game.
Being at home with the children gave me a respite from the constant bombardment of worry that I experienced when I was in-patient with her. I was relishing the sweetness of home with our other five children. Scarlett took to resting in Rini’s swing, which I found so poignant. We were preparing costumes for trick-or-treating, and the days were as peaceful as they could be under the circumstances. I remember not being overly concerned about the surgeons’ desire to order the VAD, since Rini seemed relatively stable from where I sat. Intellectually, I knew she was seriously ill. “Very medically fragile” was how her team characterized her on that day. But I was obviously sitting at the delusional table.
From October 30th, 2016
I have very few memories of this day, three years ago. But I do remember the laughter of my other children as they played, and how beautiful the fall foliage was. God had given me a reprieve and a chance to catch my breath. I would need the strength that I was rebuilding, as the darkest days were less than a week away.
From October 31st, 2016
On this day, three years ago..
From my journal:
“Up in Seattle, Rini is resting as her team has continued to struggle to find her point of stability. They are characterizing her as “extremely medically fragile,” and each day brings its ups and downs. Every day that she makes it without a major setback or catastrophic event is a victory. This limbo that our child is in is a very bittersweet place to be in. On the one hand, we are so immensely grateful that she is listed for transplant. But on the other hand, we are fearful that her chance will not come or that if it does, she will not make it through. We miss her voice, holding her, seeing her smile. But conversely, we feel incredibly fortunate that she is still here with us and that at least we still have the hope that we will have her back at some point. I miss her so much. Almost each night I have had a vivid dream about her, and as hard as it is to be away from our other children, I yearn to be back in the same room with her just so that I can look at her sweet face and touch her skin.
Child Life came by yesterday and Eric was able to order a costume for her. Today, the CL specialist came to her room and they placed her costume on top of her. Eric tucked a lollipop that he had purchased for her into her grasp so that on this, her first Halloween, she would be able to come as close as possible to trick-or-treating. Her costume is of a Pirate Princess, which I feel is most apt since she has certainly stolen our hearts.”



























Leave a Reply