I am very excited about Chinese New Year this year because I am a Rat! My high school’s mascot was the River Rat so I wholly embrace my Chinese zodiac animal. The Great Race account of the Chinese zodiac tells the story of a race across a river. As legend goes, the crafty Rat hopped on the back of the Ox and sang to him as they crossed the river but when they neared the other side, Rat jumped off ahead of Ox winning the race and was named the first animal of the Chinese Zodiac.
So as we begin a new decade in 2020, we also begin a new cycle of the Chinese zodiac.
Celebrating Chinese New Year can seem daunting, but it can also be a lot of fun – and is a great way to bring some Chinese culture and new family traditions into your home. Our celebrations may be a bit like Chinese food found in America: not quite what you find in China, but it’s what we have. And as my mom always says, “Done is better than perfect.”

We completed our first adoption from China in the summer of 2013. We celebrated our first Chinese New Year in 2014, the year of the horse. Since we had only been home six months, I am not sure how we pulled it off but we did have help. We were blessed to meet friends while in China who have become some of our best friends in life. We actually met in Beijing, on the front end portion of the trip and then spent the entire time together in Guangzhou since both of our boys are from Guangdong. Our friends live about 4 and ½ hours away but we wanted to keep up the friendship and celebrating Chinese New Year together became a tradition. Our friends come for the weekend once a year sometime around Chinese New Year depending on our schedules so we don’t always celebrate on the actual day.
One great place to get started is at your local library. Sometime after January 1st I stop by our local library and check out every book on Chinese New Year; sometimes I even request other books from libraries in our network. These books are full of information and great ideas. Some are just fun stories about Chinese New Year for elementary age children. They also can be displayed as decorations on a mantel.
One website I have found to be very helpful is called Chinese American Family. I love this site and their page on how to Celebrate Chinese New Year is full of information especially if this is your first rodeo. This site contains a lot of information including; history and folklore, activities, decorating ideas, information about red envelopes, recipes, crafts and buying guides.
I have to admit that I don’t have a Pinterest account so my friend is in charge of the decorations. I keep all of the decorations from year to year in a bin that I pull out each year when they come; we add a few new decorations each year. Since we host, I am in charge of the menu. Division of labor has helped us pull off this family celebration each year.
If you don’t have another adoptive family to celebrate with you can ask any family to join you as this is a great excuse to get together with friends and family in January or February (depending on the year) that doesn’t include football as the main theme.
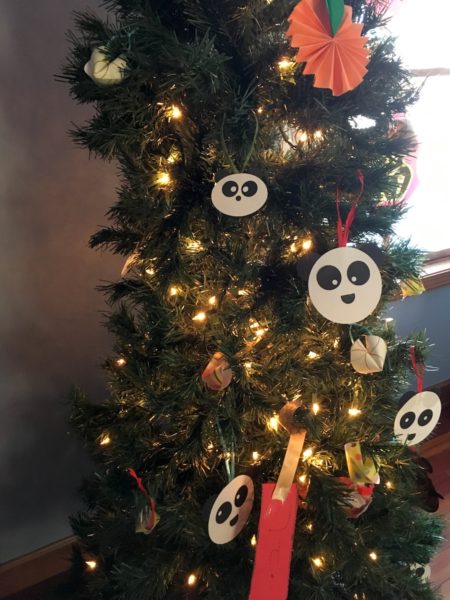
Decorations can be ornate or simple. One year we left up the Christmas tree after Christmas. We took off all of the Christmas decorations, left the lights on and added homemade Chinese New Year decorations. We made little pandas, plum blossoms, and fortune cookie decorations all out of old scrapbook paper. This was the “most ornate” year. Other years we have simply used red streamers, paper plates, napkins, plastic wear, and decorations all from a dollar store. Red, corresponding with fire, symbolizes good fortune and joy. Red is found all over the place during Chinese New Year.
A big bowl of mandarin oranges is a perfect centerpiece for your table not to mention delicious and nutritious. Mandarin oranges symbolize luck in the New Year. In China the word for a mandarin sounds similar to the word for gold and so having a big bowl of them in your home at New Year is sure to bring riches into your life or at the very least your daily requirement of vitamin C.
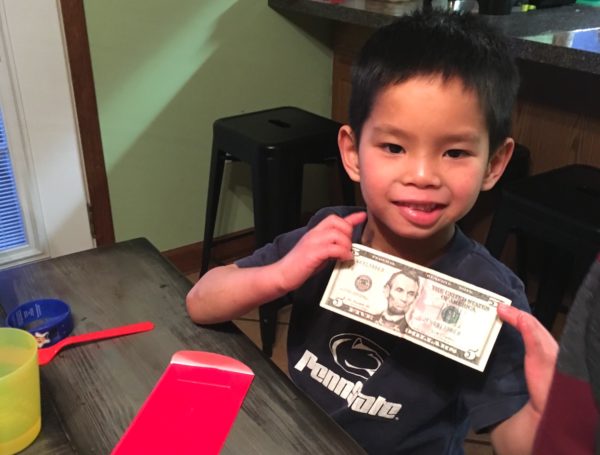
Our kids look forward to the red envelopes each year. Each child gets one at our celebration. There is a lot of etiquette surrounding the giving and receiving of these iconic envelopes filled with money at Chinese New Year. Some of the basics are that they are usually filled with new bills and not coins and in even numbers (except for the number 4 which is unlucky and sounds like the word for death). You can find these envelopes online and the amount you put in them doesn’t really matter, what matters most is the generosity of the giver and the thankful heart of the receiver. Please, thank you and hugs all around!
Chinese New Year includes traditional foods. The ones that are most common, and we find most commonly enjoyed, are dumplings, spring rolls, noodles and any golden, round citrus fruits (mentioned above). Some years we have made what I call American moon cakes using our moon cake mold and a shortbread recipe I found here on NHBO.
I know one adoptive family who gets take-out for Chinese New Year. I love this simple tradition. This is a splurge and a treat and makes for a great family tradition with a lot less fuss in the kitchen. I have to admit that this year I bought frozen dumplings and frozen spring rolls. In the past we have made our own dumplings assembly line style using store bought won ton wrappers. I want to spend less time in the kitchen this year and more time drinking coffee with our friends. The kids are growing up and have increased in number and size and somehow I have gotten older too and spending the day in the kitchen is not as alluring as it once was.
The point is that if you love being in the kitchen and that is life-giving, there are many great recipes online. If spending the day preparing a feast is not life-giving, there are so many great options out there. You don’t even need to go to a traditional Chinese market to find great dumplings and spring rolls, although a trip to one could be a great part of your tradition. I have found some great frozen options at grocery stores and warehouse stores.
One additional food item we enjoy is the “tray of togetherness”.

Traditionally this is a sectional serving platter with eight compartments (eight rhymes with the word for good luck) filled with bite sized treats such as candy, dried fruit and nuts. Each treat has a symbolic meaning and you offer these treats to guests wishing them sweet life in the coming year. It is similar to serving hors d’oeuvres. I improvise and use an old Rubbermaid tray that only has seven compartments. I use whatever small treats I have on hand or remember to pick up and we have made up our own meanings for the foods.
Red and black watermelon seeds, candied lotus root and seeds and dried sweet potatoes are not staples in my cupboard, so in the past we have used things like peanuts, cranberries, mini marshmallows, pumpkin seeds, Cheerios, M&Ms and oyster crackers. My daughter came up with meanings for each. For Cheerios she came up with the circle symbolizing eternal life in God. Even the number seven for the number of compartments in our family tray symbolizes perfection and completeness.
Over the years we have included crafts from downloading coloring pages of the zodiac animals to making paper lanterns. We have also made up some of our own games like Chinese New Year Charades and Chinese New Year Pictionary depending on the ages and stages of our children.
If you are lucky enough to have a Chinese New Year parade with fireworks and a dragon and lion dance nearby then by all means go! Here in the Midwest Chinese New Year comes at a time when the days are often cold and gray. It is a great time to make your home look festive again as it always seems to look a bit barren once the Christmas decorations have come down. It is a great time to gather with family and friends between Christmas and Easter.

Celebrating Chinese New Year is also a great way to celebrate your child’s Chinese cultural heritage. We have five kids, two of them are treasures from China, and they all love celebrating Chinese New Year. As adoptive families we are already considered “nontraditional” – our Chinese New Year traditions may not be authentically or traditionally Chinese but they are ours and they create family togetherness. They may not be Pinterest perfect but they are filled with family, friends, delicious food and well wishes for the New Year.
I hope this will encourage you to make some Chinese New Year traditions of your own.
Happy New Year! Shǔ nián xíng dà yùn!
– guest post by Tanya





































