This post is intended for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
Poop is a daily topic of conversation in our home. After three years of being in the trenches, I can tell you more than you’d probably ever want to know about it, but it hasn’t always been this way.
When we were reviewing our son’s file I was completely clueless about his special need and had never heard the term bowel management. What we did know was that there was a better than average chance that our son would need some type of bowel management in order to empty his colon regularly and achieve what is known as social continence. I know from experience that the words bowel management can be a bit scary and overwhelming for prospective and newly adoptive parents. With this post I hope to help those who are currently navigating this path and those reviewing files have a better understanding of what bowel management is.

Ultimately, bowel management is just a different way of going poop. In its most simple form, bowel management is a daily regiment for individuals which allows them to empty their bowels approximately once per day, and remain clean and accident free for the next 24 hours or until their next bowel emptying regiment. This form of continence is known as social continence. A few examples of special needs that may require bowel management include anorectal malformations (anal atresia), Hirschprung’s disease (mega colon), spina bifida, spinal cord injury, neurogenic bowel, cloaca, and cerebral palsy.
While the reasons a child may need a bowel management program are numerous and varied, the good news is that many successful treatment options exist and when used within a regular bowel management program will allow most children to achieve social continence.
For the purpose of this post I have divided the bowel management protocols into three categories: laxatives, rectal enemas, and surgical.
LAXATIVES
The first option for bowel management is laxatives. An individualized bowel management program might involve one or a combination of these medications. Commonly used laxatives for bowel management include:
- Stimulant laxatives: Stimulate the nerves in the colon and rectum which causes the muscles in the wall of the bowel to squeeze or contract and move the stool. Examples: sennosides (Senokot, ExLax) and bisacodyl(Dulcolax)
- Stool softeners: Help mix fluid into the stool to soften it. Example: docusate (Colace)
- Osmotic laxatives: Works by increasing the amount of fluid in the large bowel by drawing fluid into it causing the large intestine to hold more fluid which stimulates the bowels. Examples: polyethylene glycol (Miralax), magnesium hydroxide (Milk of Magnesia)
- Bulk-forming: Add “soluble” fiber to the stool causing the stool to absorb more water, which creates larger, softer stools that help trigger the bowel to contract. Examples: psyllium (Metamucil) and methylcellulose (Citrucel)
RECTAL ENEMAS
An enema is a procedure in which a liquid solution is inserted into the rectum to expel its contents.
- Fleet enemas: A brand of disposable, small-volume enemas that come in several forms. Fleet saline enemas work by drawing water into the colon to soften the stool to help produce a bowel movement. Fleet mineral oil enemas are a lubricant laxative that coats the fecal contents to prevent water from being absorbed out of the stool. Fleet bisacodyl enemas work by directly stimulating the intestine to increase the rhythmic action that pushes feces through the bowel.
- Suppositories: Similar to enemas in that they are inserted into the rectum, but differ in that they are small capsules or applicators containing either glycerin or bisacodyl which work to promote a bowel movement.
- Large volume balloon enemas: Consist of a preset large amount of either water or saline along with a certain amount of irritant (glycerin, castile soap, baby soap) that causes the colon to contract and evacuate the stool. Large volume balloon enemas are administered using a gravity/kangaroo feeding bag and foley catheter with balloon. The bag is hung from an elevated position and the fluid is placed in the bag. The catheter is connected to the bag tubing and is inserted into the rectum and the balloon inflated. The valve on the bag tubing is then opened allowing the fluid to slowly flow into the colon. The inflated balloon acts like a plug and keeps the fluid from leaking back out. When it is time to release the fluid the balloon is deflated and the fluid and stool are expelled. (administration video)
- Large volume cone enemas: Similar to the balloon enemas in that they consist of a fluid bag, tubing, a large volume of saline or water, and an irritant. The difference is instead of a balloon catheter, a plastic cone shaped tip is used. The cone is inserted into the rectum and the fluid permitted to flow in. The cone acts as a stopper to keep the fluid in the colon until all of the solution has flowed in, at which point the cone is removed and the fluid and stool are evacuated. (administration video)
- Peristeen anal irrigation system is similar to large volume balloon enemas in that it uses a large volume of fluid, a specialized catheter with a balloon, tubing, and a bag. The Peristeen does not however rely on gravity to introduce the fluid into the colon and instead uses a pump system. Unlike the other two types of large volume enemas the Peristeen system is designed to work with water alone removing the need for added irritants. (Peristeen informational video)
SURGICAL
Malone Antegrade Continence Enema (MACE, Malone, ACE, appendicostomy)
An appendicostomy, or Malone, is just another way of administering an enema that is done for children who need an enema every day to stay free from stool accidents and. A Malone procedure (MACE), is a surgery that makes a pathway from the colon to the belly button or other location on the abdomen. With the Malone procedure, the enema is given from the beginning or top of the colon via the created pathway, instead of up trough the rectum, and stool is evacuated from the rectum with the enema fluid. This type of flush is essentially from the top down, rather than bottom up.
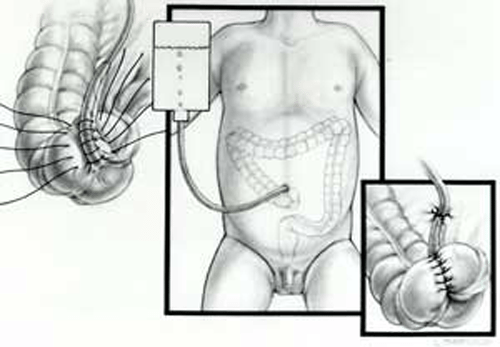
The surgeon connects the appendix to the belly button (umbilicus) or right corner of the belly (abdomen), and a one-way valve is created inside the child’s abdomen. This valve allows the enema tube (catheter) go in, but no stool or body fluids will be able to come out. Often, if the procedure is done using the belly button the valve is not visible. The surgeon makes the valve with the child’s natural tissues and skin and no artificial device is used. The Malone tube (catheter) can be inserted through this valve. The solution can be flushed through the new valve the same as a rectal enema. (source: Nationwide Children’s Hospital)
Sacral Nerve Stimulation (SNS, or Sacral Neuromodulation)
Sacral nerve stimulation is a promising new therapeutic modality for pediatric urinary and fecal incontinence, and chronic constipation in children when other treatments have been unsuccessful. The technology can be compared to a pacemaker for the heart, but instead, it provides stimulation to the anal canal area, lower part of the colon, and the bladder.
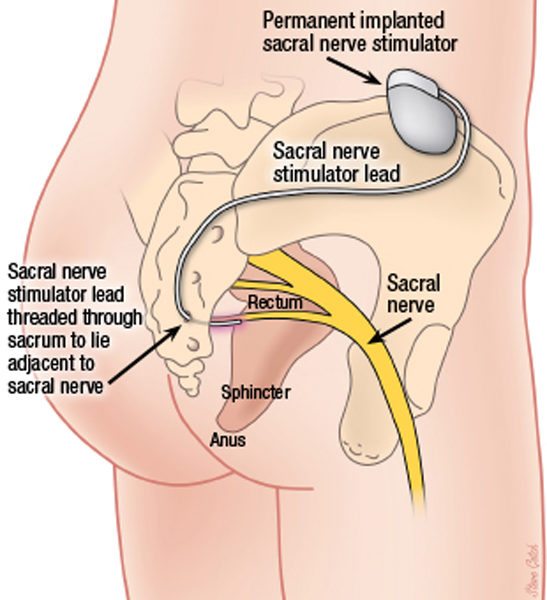
Sacral nerve stimulation is a two-stage procedure that involves a test phase, where the child is closely monitored, and if significant improvement is observed, is followed by permanent implantation of the electrical stimulator. Members of the care team continue to monitor the patient’s progress as he or she reintegrates into daily activities. The implanted device addresses communication problems between the brain and the nerves by delivering mild electrical impulses to the pelvic nerves. The pelvic nerves, in turn, begin to tell the muscles when to contract, ultimately helping control the ability to urinate or have a bowel movement.
In addition to helping children with urinary and fecal incontinence, and chronic constipation, sacral nerve stimulation has proven successful in some children with anorectal malformations, Hirschsprung disease and certain forms of spina bifida (source: Nationwide Children’s Hospital).
PEDIATRIC BOWEL MANAGEMENT PROGRAMS
Nationwide Children’s Hospital (Columbus, OH)
Children’s Hospital Colorado (Denver, CO)
Seattle Children’s Hospital (Seattle, WA)
Boston Children’s Hospital (Boston, MA)
Cincinnati Children’s Hospital (Cincinnati, OH)


























Leave a Reply